Print version
Search Pub Med
Novel anti-thrombotic role for PPARβ in human blood
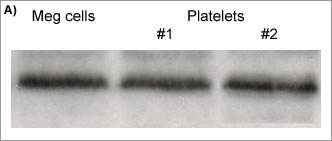
Prostacyclin is formed by the consecutive actions of cyclooxygenase (COX) and prostacyclin synthase in the endothelium. It exerts its effects by actions on cell surface prostacyclin (IP) receptors linked to activation of adenylyl cyclase. However, prostacyclin is also a ligand for the nuclear receptor peroxisome proliferator-activated receptor beta (PPARβ ; Lim & Dey, 2002). Prostacyclin is a powerful inhibitor of platelet aggregation, an effect that has been attributed to activation of IP receptors. Here we have studied the potential for PPARβ activation to influence platelet function. Human blood was collected by venepuncture into citrated tubes (0.109 M) and responses measured using electrical impedance aggregometry. Aggregation was also measured in platelet rich plasma using light transmission aggregometer. Aggregation was induced by addition of ADP (10 µM) with maximal responses being recorded after 15 min. Platelet progenitor cells, megakaryocytes (Meg-01), were used as controls. Western blot analysis was performed using standard techniques. Figure (A) Western blot for PPARβ in Meg-01 cells and platelets from 2 donors. (B) Effects of GW0742 (GW) on whole blood platelet aggregation. (C) Synergistic inhibition by GW0742 and SNP of whole blood platelet aggregation. Data is mean ± sem for n=5-7. *p<0.05 by (B) one sample t-test and (C) two way ANOVA.
PPARβ protein expression was detected in Meg-01 cells and in human platelets. GW0742 inhibited aggregation of whole blood in a concentration-dependent manner, (e.g. 40µM inhibited ADP-induced aggregation by 70%; Figure B), and synergised with the NO donor sodium nitroprusside (SNP) (Figure C). GW0742, 40µM, also inhibited aggregation in platelet rich plasma by 58%±10 with 1 µM ADP (n=6). These observations are the first to establish PPAR β as an anti-platelet target and suggest that it may mediate some of the effects (e.g. synergy with NO) of prostacyclin on platelets. They also demonstrate that, like PPARγ , activation of PPARβ can have non-genomic acute effects in blood. Lim, H and Dey, SK (2002), Endocrinology 143: 3207-3210. This work was funded by the Joint Research Board of St Bartholomew’s Hospital, London. |